future health africa:
TRAUMA TEAM
OUR WORK
FHA Trauma Team started in 2009 (then called Kenya Orthopaedic Project) to help provide free surgical care for patients with broken bones and traumatic injuries in rural Kenya. We seek to work collaboratively with hospitals to enhance the delivery of trauma and orthopaedic care and services.
Why is the Trauma Team needed?
Skills shortage – Skills in Orthopaedic trauma and limb reconstruction within the Government sector are sparse throughout many parts of Africa.
Financial environment – Orthopaedic surgery is expensive, and with an average wage of £1 per day, many patients with traumatic injuries just cannot afford the necessary treatment and are left with permanent pain and disability, often no longer able to provide for their families.
The work is not being covered by other charities – Orthopaedic partnerships with low income countries are not common due to extremely high costs and difficulties in finding, financing and transporting instruments and specialist equipment.
Future Health Africa’s vision is ‘Sharing skills, transforming lives’. We believe that creating a sustainable trauma and orthopaedic service is key to improving the health of the local population. We are committed to two-way teaching and learning in all our projects. This is achieved by working side by side with the doctors, nurses and other healthcare professionals sharing and transferring mutual skills.
CATEGORISING OUR ACTIVITY
Trauma Team activities are categorised into Bronze, Silver and Gold activity levels. All services are delivered at the highest standard, with improving quality as a central aim.
Bronze: Providing immediate and direct patient care
Offer high quality consultations, advice and where appropriate, both operative and non-operative treatment for patients referred to us.
Silver: Facilitate learning opportunities/new skills for the future
Side by side working with exchange of knowledge and skills
Develop a safer surgical environment.
Anaesthesia: Exchange knowledge on safe anaesthesia, regional anaesthesia and pain management
Gold: Trauma service sustainable improvement/development
Identify areas to develop a stepwise pathway
Support local need and wishes to change
Develop non-operative treatment options for local patients
Ongoing support and communication outside of projects
We typically spend six days working with the local hospital team to see patients for consultations, to perform surgical operations and to provide physiotherapy or give advice. Almost all the patients we treat have had an injury which has not healed properly and has left them with a disability. Often these patients are unable to walk or use an arm. We have placed a strong emphasis on continuous rehabilitation, follow-up and audit of practice to ensure safe and effective patient management.
OUR PARTNERS
Our current partner hospitals:
Nyahururu District Hospital
Marsabit District Hospital
Previous partner hospitals
Kitale District Hospital
Nanyuki District Hospital
Coast General Hospital
Anaesthetist Will Jewell with 64 year old patient Koder, after a successful hip operation. Nyahururu, 2015
Deep concentration: Surgeons working closely together.
PATIENTS
Here are just a few of the many patients that we have treated. For more examples of FHA project successes, please visit our Case Studies page.
“Fixing one person will influence a whole family, even a community. ”
Ahmed
Ahmed is 53 years old and had an open fracture of his shin bone ( tibia ) 3 years ago. He had an operation 3 years ago in Ethiopia to fix the fracture with a rod in the centre of the bone. The rod broke leaving him with a fracture that had not healed and made it difficult for him to walk at all. We fitted him with an aircast boot and he was so happy with this that he did not want further surgery. The Aircast boot was recycled from a UK fracture clinic. In the UK they are used by a single patient and then thrown away.
Ayub
Ayub is a retired gentleman and a year before we met him he had an operation to fix a broken right knee cap. The knee did not recover well and unfortunately became very stiff. It was stuck in an almost completely straight position. For him this made it impossible to kneel to pray, use public transport easily or climb hills or stairs easily. We were able to operate and remove the scar tissue from the knee. Here at the end of the operation you can see how well the knee moves and a few days later Ayub was able to start using the knee more normally.
Hamitha
Hamitha was 11 when we met her. She had injured her left elbow 6 months before and broken the humerus bone. Sadly the elbow did not recover well and she was left with a very stiff arm with the elbow stuck in an almost completely straight position which did not allow her to get her hand to her mouth or do any of life’s normal tasks with it. We were able to operate and remove the scar tissue from the elbow allowing her to begin to use the arm more normally again.
HOW YOU CAN HELP
Donations
The financial cost of Orthopaedic surgery is prohibitive for most patients and their families.
Many patients are not able to pay for surgery which would give a child the chance to walk or enable a parent to return to work and provide for their family.
The cost of each of our Trauma Team project visits is approximately £16,000. Travel and accommodation costs for volunteers makes up 75% of that figure (and is mostly raised through fundraising by individual volunteers), whilst provision of equipment, implants and drugs makes up the remaining 25%.
Would you like to make a difference in the life of someone in need? Why not consider helping a needy patient today by donating towards an Orthopaedic implant. The impact of your donation would transform the life of someone in desperate need. Your donation could help to buy:
An Implant to fix a child’s broken femur or tibia (£20)
A surgical wire to stabilise a child’s broken elbow (£10)
A standard plate and screws for fracture fixation (£30)
External fixator rods and clamps which will be used repeatedly for fracture fixation (£400)
The reusable instruments needed to implant a bone plate (£500)
DONATIONS can be easily made via kind link at https://donate.kindlink.com/Future-Health-Africa/4942
Volunteer with THE FHA Trauma Team
Our volunteering ethos – all volunteers donate their time and contribute financially to the delivery of the project. All members work closely together to deliver the highest quality of care.
A typical Trauma Team includes professionals such as Orthopaedic Surgeons, Anaesthetists, Theatre practitioners, Radiographers, Physiotherapist as well as a coordinator.
We usually carry out two Trauma Team projects every year, each lasting 10 days.
There are also opportunities to volunteer in the UK to help with the large amount of work required to run the project.
If you’re interested in volunteering, please contact traumateam@futurehealthafrica.org
Visit our volunteer page for the handbook and agreement volunteer documents
Organise or participate in a charity fundraising event
Hippo attack patient Lopoe wearing a knitted hat donated by charity supporter, Marie Dempsey. Nov 2016
THE MULTI-DISCIPLINARY TEAM
Anaesthesia
Without anaesthesia there is no surgery! Access to safe surgery goes hand in hand with safe anaesthesia and is a human right.
We work with local Anaesthetists to develop and improve local services through listening and learning. Regional anaesthesia is a particular area that with development can provide safe, pain free anaesthesia and post-operative analgesia. This can best be achieved by the use of ultrasound.
We take trainee Anaesthetists from the South West with the aim of two way exchange in ideas and teaching. We recognise training the new Anaesthetists of the future in both countries provides benefits to all. We hope to inspire others into the profession as there is a massive shortage of Anaesthetists across all low and middle income countries.
Surgery
Patients who need an operation for their fractured bone often cannot afford to pay for the surgery. Even if they can afford it they often have to travel long distances to have their broken bone assessed.
We work side by side with Kenyan surgeons nurses and junior doctors to exchange knowledge and skills. Where possible we donate implants such as the plates and screws needed to fix a broken bone so that patients don’t have to pay. We don’t charge fees for our work. We will try and let nature heal fractures without surgery but some fractures will simply not heal on their own leaving patients severely disabled.
Doctors who are training to be specialists in trauma surgery join us from the UK and Kenya for our visits. On average we will provide an assessment for around 300 patients and will operate on 20-30 patients a week.
Using an Image Intensifier in Theatre
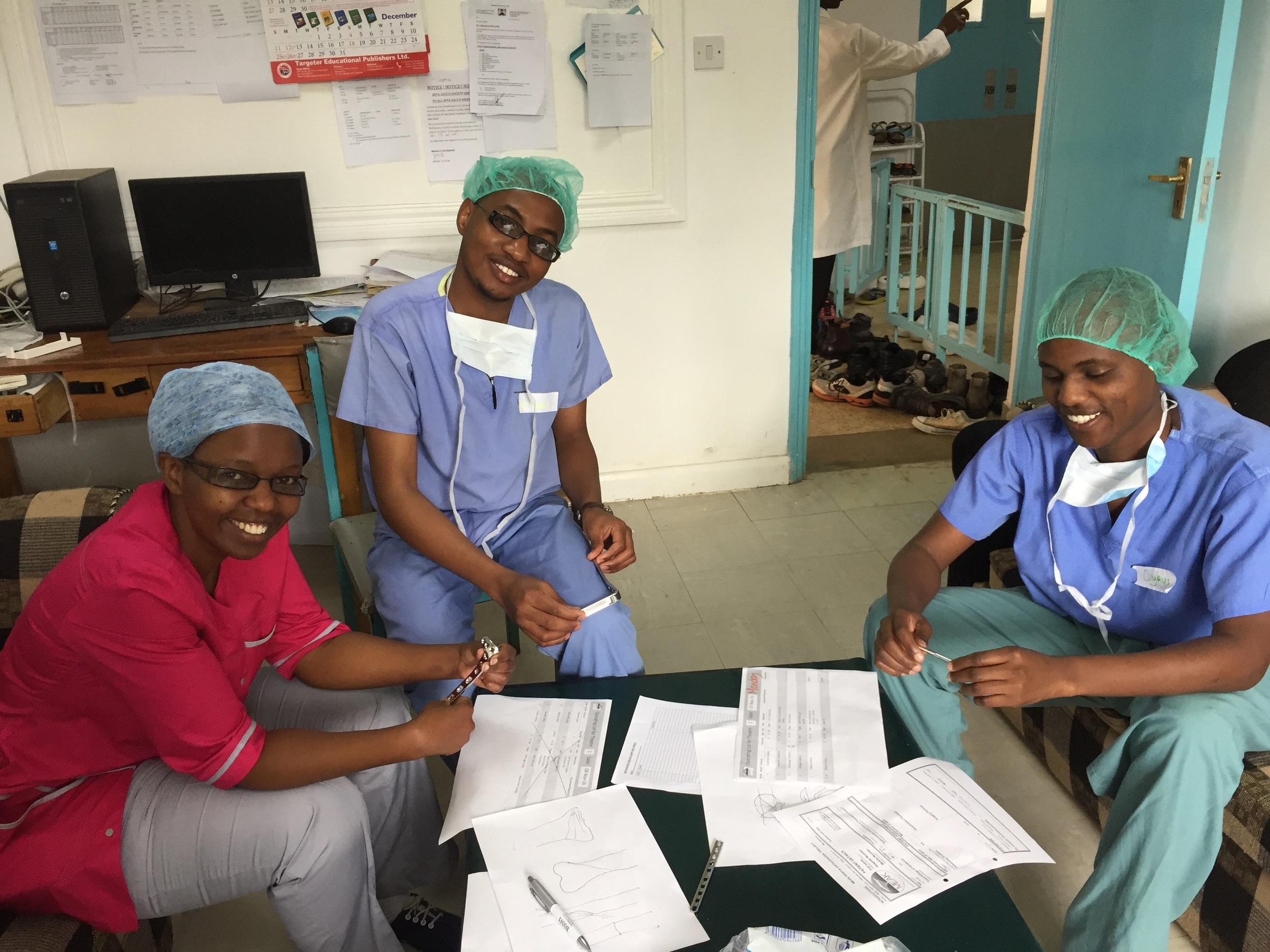
Lots of smiles from the theatre staff at the end of a hard day of surgery. Marsabit, Nov 2018
Radiography
The radiographer on the team looks after the medical imaging needs of the orthopaedic surgeons primarily. This will sometimes involve ensuring that the patients have had the correct images taken before an operation can be planned, or taking images after the operation to ensure that everything is in the right position to heal correctly.
We also have an important part to play during the operations themselves. Using a machine called a Mobile Image Intensifier it is possible to take live, real time, x-rays in theatre whilst the patient is being operated on. This means that the surgeons can be certain at the time they are operating that screws, nails and plates etc are correctly sized and positioned and that the fragments of bone are in the right place and in alignment. This massively helps to reduce the risk to the patients of the long term effects of poorly healing breaks, and badly aligned limbs.
During both of these roles we like to work alongside the local Radiography Staff, teaching them techniques they may not have seen before, and learning from them ideas and procedures for getting the best out of the limited resources that they have.
Theatre team
The theatre team consists of registered practitioners who are Nurses or Operating Department Practitioners, and also includes Theatre Health Care Assistants with an interest in orthopaedic and trauma theatre environment, providing teamwork and knowledge in the scrub and anaesthetic practitioner roles. Emphasis is based around the knowledge and skills exchange within the partnership of the local team, by working together side by side, facilitating the goals of helping to create a trauma service for their hospital and community.
Working side by side is a great opportunity to get to know our new friends and colleagues with similar roles, making an engaging setting to enable learning of new surgical and anaesthetic techniques they may not already be familiar with. It also provides reassurance and encourages good practice by promoting and contributing to a safe surgical environment set out by the World Health Organisation and the Lancet Global Surgery.
PROJECT LEADS
Darren Munn,
Theatre Team Lead / Project Coordinator
I am a Surgical Care Practitioner in Trauma & Orthopaedics at Torbay hospital in South Devon, UK and I am also a Registered Operating Department Practitioner. I started volunteering for the charity in 2012 and have taken on many roles within the surgical, anaesthetic and management team.
Volunteering has been so rewarding for me! Being able to help individual patients, teach and help and learn from our African colleagues, whom I am proud to call friends, facilitate the change that they strive for.
Volunteering has made me more appreciative, put a better perspective on personal and professional matters and learn to become more adaptive from an environment that is not as privileged.
If you are thinking about volunteering,
do it!
Will Jewell,
Lead Anaesthetist
I am a Consultant in Anaesthesia and Intensive Care Medicine working at the Royal Cornwall Hospitals Trust where I have held the post since 1998. I joined the Trauma Team in 2015. I have been Lead Anaesthetist for the Trauma Team since 2016.
I have particular interest in regional anaesthesia using ultrasound, peri-operative care pain management and paediatric anaesthesia. I teach at University of Exeter Medical School.
I have a passion for global health and helping those whose access to healthcare is not a given, as it is for us. I am a keen cyclist and have two spaniels and eight chickens.
Christoph McAllen,
UK-based Trauma Team Lead Surgeon
Consultant Trauma & Orthopaedic Surgeon, University Hospitals Plymouth, UK and Visiting Lecturer at the University of Nairobi Department of Orthopaedics.
My first visit to Kenya as an Orthopaedic surgeon was in 2011. Since then I have returned for one or two visits per year. Each year and each visit brings new challenges and rewards.
I value the new friendships both professional and personal that these trips have given me. When back at home in my day job in Plymouth I can draw on my experiences in Kenya and I know that my patients in the UK benefit from that.
Trauma Team is developing fast. If you want to be a part of it please get in touch!
Dr Samuel Ndanya
Kenya-based Trauma Team Lead Surgeon
I am an Orthopaedic & Trauma Surgeon in Laikipia, Kenya. In 2008 whilst a surgeon at Nanyuki District Hospital, I met Dr Lucy Obolensky from Torbay in Devon. Lucy had been helping to improve access to primary healthcare for Maasai communities in Laikipia and Samburu areas of the Rift Valley in Kenya since 1997.
I asked Lucy if she could organise an orthopaedic trauma project to come from the UK to Nanyuki District Hospital. This first trauma project led to the formation of a partnership with Torbay Hospital and the charity Future Health Africa. I continue to work closely with the charity as the Kenyan Trauma Team Lead Surgeon.
Dr. Mary Nduta Kibote, Kenya based Trauma Team lead
I wanted so much to be a doctor that I took myself to the Ukraine to study for 6 years (as there were limited opportunities in Kenya). Learning Russian and Ukrainian was a big challenge but I succeeded. The charity supported me and now I am back in Kenya trying to improve healthcare here.
Through my undergraduate, internship and now as a registered doctor in Kenya, working as a volunteer in this charity, I have learnt many new surgery skills and also how to be a good team player. The work I have done with Future Health Africa has really helped me increase my confidence to work independently with minimal supervision
I believe FHA is one of the world’s best charities as it provides a broad range of well-organised clinical approaches and experiences. It also leaves behind successful sustainable qualitative operation programs and management. I value the opportunity of working with such a charity.
Alice Inman, Lead Physiotherapist
I’ve been a physiotherapist since 1996. I started doing voluntary health work as a student and have not really stopped. It’s been the most rewarding aspect of my career and taught me so much, clinically and personally, let alone learn about other cultures across the globe.
I have been involved with the Orthopaedic Projects in Kenya since 2011 and just love the team approach and the partnerships/ friendships we have formed within UK and Kenyan Colleagues. The Kenyan people are so warm and friendly and it’s always a total delight to work with them. It makes me very humble about all the opportunities and resources i have back at home.
My overseas volunteering has influenced my career back in the UK to the point that I am now the academic lead of the MSc Global Health at the University of Plymouth. It’s really great to be able to encourage and support other health care professionals on their journey’s into Global Health. It’s so rewarding and is gaining more and more recognition into its role for the future of the NHS. If you’ve any inkling that you’d like to volunteer abroad I’d be the first to say “Go”!
Tim Cooper, Radiography Lead
I am a diagnostic radiographer with over 30 years experience in the NHS, currently working at Torbay Hospital. My main responsibilities in Torbay are looking after education and Continuous Professional Development for student radiographers and qualified staff in the department. I also have an interest in Orthopaedic Theatre Radiography and help with training and assessment of theatre skills for undergraduate students and newly qualified staff.
This mix of interests and experience has been perfect for my trips to Kenya with the FHA. My role on the trips is two-fold:
Firstly I provide real-time live radiographic imaging for the orthopaedic surgeons as they operate and put all manner of screws, nails, pins and plates into broken bones to aid healing and reduce pain. X-rays are used to ensure that all the metal work is the correct size, and the alignment of the fractures is made as good as possible.
My second role is an educational one; encouraging local staff get involved with the operations as much as possible, giving them tips and pointers so they can get the best possible images, and also more formalised teaching around topics such as image interpretation and radiation safety in operating theatres.
Between trips I get involved with fundraising for the charity and with recruitment of other radiographers to work with the team.
I have always gained a great deal from my trips to Kenya, meeting professionals who achieve so much with so little support. There’s a massive sense of achievement from the life changing treatment we provide to patients, and from knowing that some of the ideas and techniques I pass on whilst there can carry on helping people into the future. On returning home from Kenya, I am always struck by just how lucky we are in the UK to have the NHS, even when it is struggling and can seem far from perfect.
Debbie Lannon, Admin Lead
I have volunteered with the Charity since 2012 and have been to Kenya on eight projects to four different hospitals. I am usually the only non-clinical role on the Trauma Team projects and my main tasks are to record all patients on the database, create theatre lists, type up surgery notes, update our social media pages and generally ‘muck in’ wherever I can help.
Prior to the trips, I help with booking flights, accommodation and transport to and from the airport, as well as booking trips for R&R time. I also help out with admin for the charity back in the UK.
There’s no hierarchy on these projects; every member of the team is valued for their role, and as well as hard work there is also lots of fun and friendship; I have made many friends with both African and UK colleagues over the years.
Working in a foreign country, without the usual comforts of my own office and the back-up of an IT team, has taught me to improvise and has made me more resilient. I’ve learnt a lot about global health and different cultures and I’ve gained a real appreciation for the NHS.
If, like me, you are non-clinical and think you wouldn’t have a role to play in a healthcare project, think again! There is always plenty of non-clinical work to do. Give it a try!
GALLERY
Below: Our work at Kitale, Nyahururu, Marsabit & Nanyuki District General Hospitals since 2013





















PUBLICATIONS, PRESENTATIONS AND GOVERNANCE
For details of our publications, presentations and research, please visit the Future Health Africa Outcomes page.
Trauma Team follow the FHA Governance guidelines, which can be viewed here.

















